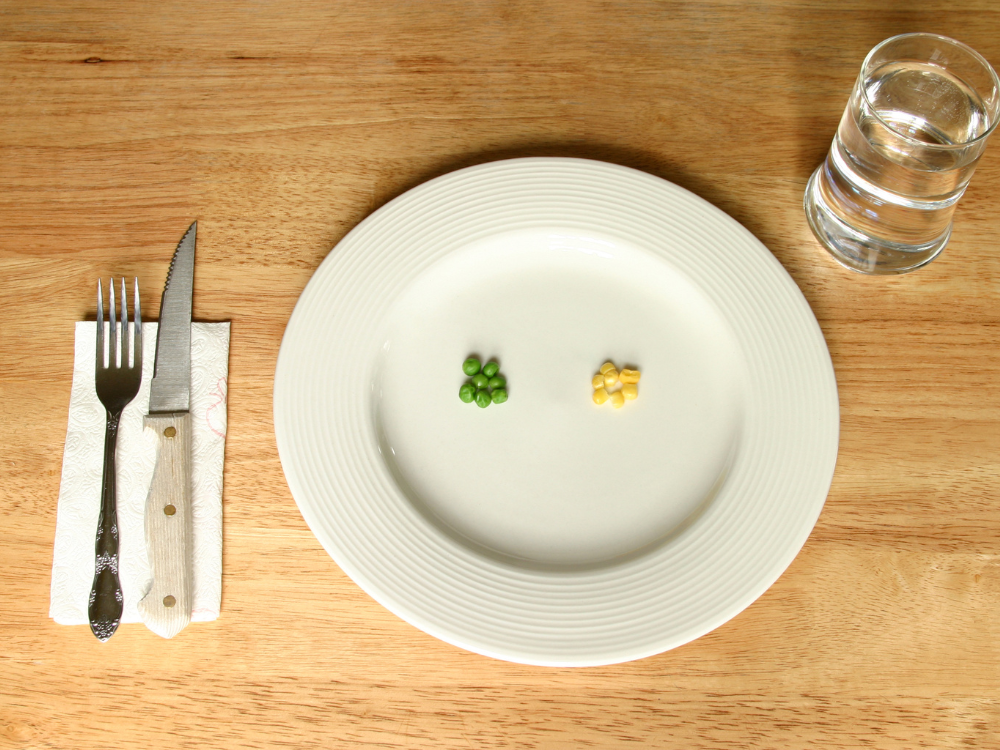
Disordered eating behaviors, such as binge eating, emotional eating and restrictive dieting, often coexist with obesity, creating a vicious circle that complicates efforts to achieve and maintain a healthy weight. Binge-eating disorder and body dysmorphic personality disorder are the most common disordered eating behaviors correlated with obesity. However, anorexia nervosa has the highest chance of mortality.
The relationship between obesity and disordered eating behaviors represents a complex combination of psychological, physiological and environmental influences.
As obesity rates rise across the world, understanding this connection has become increasingly important in addressing the disease.
Disordered eating behaviors, such as binge eating, emotional eating and restrictive dieting, often coexist with obesity, creating a vicious circle that complicates efforts to achieve and maintain a healthy weight. Binge-eating disorder and body dysmorphic personality disorder are the most common disordered eating behaviors correlated with obesity. However, anorexia nervosa has the highest chance of mortality.
An estimated 9% of the U.S. population will have an eating disorder in their lifetime. The prevalence of disordered eating behaviors is seen to be higher in women, but it can also impact men and adolescent age groups. Exploring the influences between these behaviors and obesity reveals not only the challenges individuals face but also the necessity for integrated, compassionate approaches in treatment and prevention.
Obesity and disordered eating have a parallel linear relationship, but this relationship has not been discussed enough, even though it is a public health concern. As chronic stressors escalate, the balance of self-regulation within the brain-gut axis is increasingly disrupted, underscoring the complexity of this association. Studies have shown that disordered eating behavior is prevalent in patients with a higher BMI. However, one can develop disordered eating behavior at any weight and stage of life. Acknowledging this dynamic is paramount for devising strategies to address both obesity and disordered eating effectively.
Disordered eating behavior is diverse, complex and multifactorial. Most people who have obesity do not have an eating disorder, but eating disorders are more common in people living with obesity, and there is significant overlap between the two. Societal attitude, lack of support, ethnicity, weight bias and stigma in the workplace, at home and in health care settings play a significant role in impacting mental health in patients with a higher BMI. From bulimia to anorexia to restrictive eating patterns, they can all happen in continuum while being commonly missed in practice. Patients often avoid disclosing their behavior to family or health care providers because lack of self-esteem and social stigma.
When treating disordered eating behaviors in patients with obesity, the first step is to address mental health. No obesity treatment can be effective without untangling the mind map and building trust with patients to bring forward the ongoing challenge of eating behaviors.
Listening and motivational interviewing is one of the most important strategies used in obesity management to promote self-ownership. Optimal behavior therapies are effective when we adapt the focused approach in cognitive restructuring, stimulus control, self- monitoring and social support. It is also important to make collaborative team effort by working with nutritionists, psychiatrists and therapists.
The most effective strategies that have helped in addressing both obesity and disordered eating are cognitive behavioral therapy, interactive technologies and pharmacotherapy. Weight loss medications must be given with precaution and under supervision for patients with bulimia nervosa.
To promote a balanced and healthy weight, it is important to understand eating behavior patterns. Understanding a patient’s motivation and behaviors is critical for obesity medicine specialists to improve the overall health of the patient. The multidisciplinary approach where we work in a team of health coaches, nurse practitioners, psychologists and nutritionists is also very useful in managing patients with combined disorders.
The dynamic between obesity and disordered eating behaviors further proves the multifaceted nature of the disease of obesity. By recognizing the complexity of this relationship and adopting holistic and effective strategies to intervention, we can strive toward promoting not only physical health but also psychological well-being in patients.
For clinicians looking to learn more about obesity and disordered eating behaviors or mental health, the Obesity Medicine Association offers a variety of resources, including the Obesity Pillars journal, online webinars and the Fundamentals of Obesity Treatment Virtual Course offered three times a year.
Reference:
- People with higher weight. https://nedc.com.au/eating-disorders/eating-disorders-explained/people-living-in-larger-bodies-and-eating-disorders/. Accessed June 6, 2024.